Psoriasis: Causes, Symptoms and Treatment
Plaque psoriasis, which demonstrates well-demarcated, red plaques with a classic silvery scale.
Credit: DermNet NZ
What is psoriasis?
Psoriasis is a persistent inflammatory skin condition marked by well-defined patches of red, thickened, scaly skin. These areas can be itchy, dry, and localized to specific parts of the body or more widespread. Psoriatic lesions may also exhibit painful cracks or fissures. While these lesions tend to be long-lasting, with proper management, their appearance and symptoms can be significantly improved. However, permanent resolution of the condition remains elusive.
What causes psoriasis?
Psoriasis results from an abnormally accelerated proliferation of skin cells. Though it stems from a combination of factors, its development is primarily tied to irregular immune responses. Potential triggers or factors that might exacerbate psoriasis include:
Genetic predisposition or family history
Obesity
Smoking habits
Excessive alcohol consumption
Infections, such as streptococcal tonsillitis
Physical injuries, including cuts, burns, or tattoos
Significant life stressors
Reaction to certain medications, including lithium, beta-blockers, antimalarials, and NSAIDs
Abrupt cessation of steroid medications like prednisone
What are the symptoms of psoriasis?
Psoriasis manifests in diverse ways depending on its subtype. It typically appears as symmetrically distributed red, raised patches with clear borders, topped with a silvery-white scale. The affected areas can range from mildly to severely itchy, leading to potential skin thickening. Frequently affected regions include the scalp, elbows, and knees. The various subtypes of psoriasis exhibit specific symptoms:
Plaque Psoriasis: Predominantly appearing on the scalp, elbows, knees, and lower back, this is the most prevalent form and can sometimes be treatment-resistant.
Guttate Psoriasis: Identified by numerous small plaques, often following a streptococcal infection. Typically, it resolves within a few months.
Inverse Psoriasis: Occurs in body folds and genital regions, presenting as smooth, well-defined red patches.
Sebopsoriasis: Displays characteristics of both psoriasis and seborrheic dermatitis.
Palmoplantar Psoriasis: Specifically targets the palms and soles, leading to skin thickening and fissures.
Nail Psoriasis: Affects nails, causing discoloration, pitting, and separation of the nail bed.
Psoriatic Arthritis: Chronic inflammatory joint condition often associated with skin and nail psoriasis.
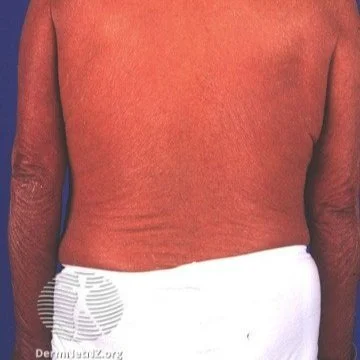
Erythrodermic Psoriasis: A rare, severe form, leading to a widespread peeling red rash. It may follow another type of psoriasis, often seen post steroid withdrawal, and is considered a medical emergency.
How do I treat psoriasis?
Managing psoriasis involves a comprehensive approach, with treatment options varying based on disease severity:
Lifestyle Measures:
Minimizing smoking and alcohol consumption
Weight loss, especially if overweight
Topical Solutions:
Emollients or moisturizers
Keratolytic products
Salicylic acid preparations
Vitamin D analogs (e.g., calcipotriol)
Anti-inflammatory creams like tacrolimus or pimecrolimus
Topical retinoids, including tretinoin and adapalene
Systemic Interventions:
If you are seeking professional advice or treatment for psoriasis, consider reaching out to a dermatologist for expert care and personalized treatment options.
Oral agents such as methotrexate, cyclosporine, and acitretin
Biologic treatments, targeting specific immune responses, including TNFα, IL-12/23, and IL-17 inhibitors
Nail psoriasis, which shows distal onycholysis (lifting of the nail plate), and oil spots (yellow spots where the psoriasis is in the nail bed).
Credit: DermNet NZ
An example of inverse psoriasis, which manifests as red, smooth patches in body folds such as the gluteal crease or underneath the breasts.
Credit: DermNet NZ
An example of erythrodermic psoriasis, which shows up as a sunburn-like rash on the whole body or almost the whole body.
Credit: DermNet NZ